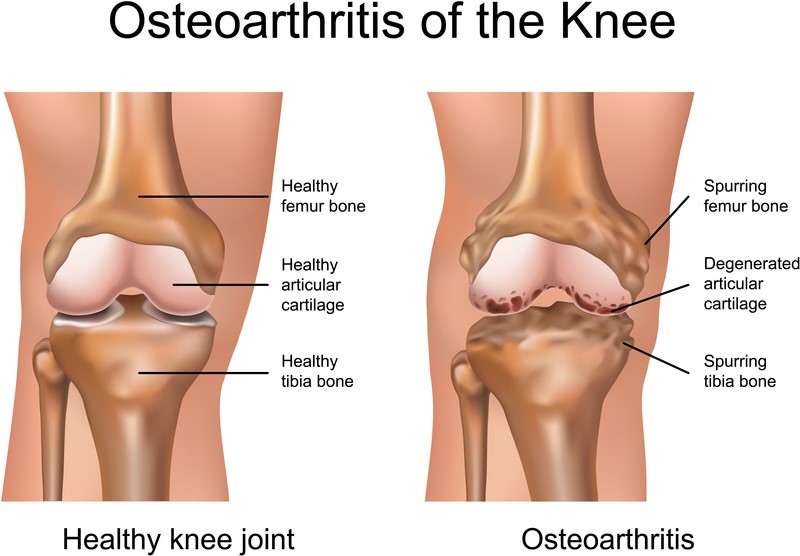
Knee Osteoarthritis is very common. It is the wearing out of the cartilage that covers the bone inside the joint. When bone rubs on bone it becomes painful. Knee osteoarthritis presents with pain around the knee, often just on the inside of the knee, but can be both sides or in the front of the knee. The knees can be straight or angled, with the knees going outward (genu varum) or the knees coming together with the feet going out (genu valugum). Pain is usually felt in the mornings, after activity, or commonly when going up or down stairs. The knees can become swollen and stiff often not being able to straighten or bend all the way. Non-operative management include anti-inflammatories such as ibuprofen, voltaren / diclofenac, and tramadol. In some people glucosamine, chondroitin, acupuncture, therapy and chiropractics may help. However like osteoarthritis of the hip, none of these change the arthritis in the knee and the knee will continue to degenerate. Often steroid injections into the knee can help in the early stages.
Knee Arthritis: http://orthoinfo.aaos.org/topic.cfm?topic=A00212
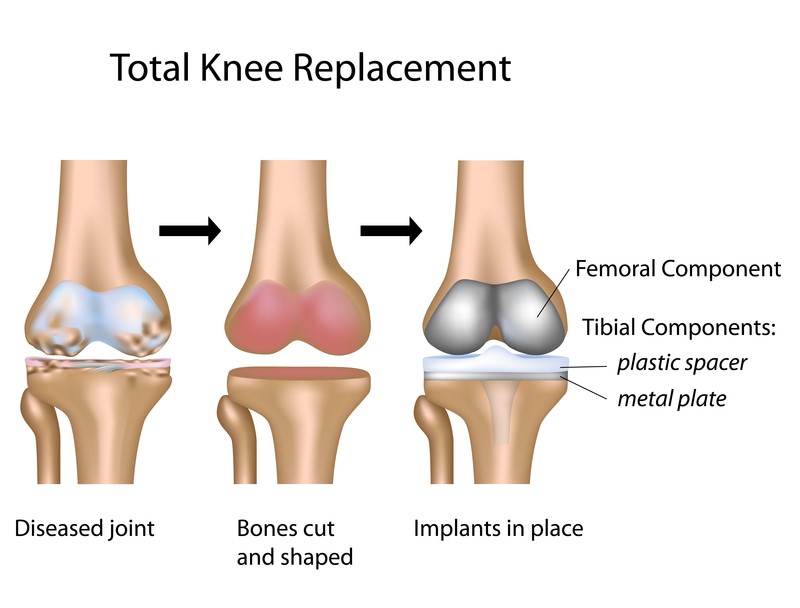
Knee Replacement
Knee replacement are increasing at a much greater rate than total hip replacements and are quite similar. There is a skin incision in the front of the knee. The distal end of the femur is removed and the proximal (top) of the tibia is removed and replaced with metal. Then a polyethylene (plastic) liner in between. The patella (knee cap) may or may not be replaced, depending on multiple factors.
Patients can expect to stay 2-5 days. Therapy begins the day of surgery with bending of the knee. Knee replacement surgery is known to be very uncomfortable surgery, especially because of the therapy required post-operatively. A knee normally takes longer than a hip to reach its maximum, which is about 1 year.
Post-operative
- Antibiotics
You will routinely be given 3 doses of antibiotics 8 hours apart, the first dose is just before the skin incision.
- Anticoagulation
A total knee replacement puts you at risk of having a blood clot in the calf, which can go to the lung causing a PE (pulmonary embolus) and can make you very sick. There is a large debate that has been going on for many years about what is the best way to prevent blood clots. The stronger the medication, there is less likely to be a clot, but much higher chance of a complication. With no prophylaxis approximately 37% of people will develop a deep vein thrombosis (clot) in the calf, however most of these will be asymptomatic. There is no difference in fatal PE’s between any of the medications. Warning signs of a blood clot are pain and/or swelling below you knee, unrelated to your incision. Warning signs of a PE are, chest pain and shortness of breath. If these occur immediately seek medical attention. To give the best protection to all my patients, I use the “American Academy of Orthopaedic Surgeons Guideline on Preventing Thromboembolic Disease in Patients Undergoing Elective Hip and Knee Arthroplasty”, for prophylaxis in all joint replacement patients, as can be found here: http://www.aaos.org/research/guidelines/VTE/VTE_summary_of_recs.pdf
- Pain relief
You will start with pain medication, through an IV line in your arm. The pain medication does very well for the pain, however it often makes you feel nauseated and constipated. You will routinely be given stool softeners to help along with anti-nausea drugs. These will then progress to oral medication, which you will go home on.
- Activities in Hospital
The first few days after surgery can be uncomfortable and for some they can feel drained. It is of vital importance that you are mobile both in and out of bed. There are many exercises that you can do whilst in bed, to speed up your recovery. Here is a link to exercises you will do in hospital:
http://orthoinfo.aaos.org/topic.cfm?topic=A00301
- Discharge home
The average patient stays between 2-5 days. Some people take a little longer which is ok and should not be seen as a cause for concern. The earlier you can get up and become independent the lower your chance of some complications and the better you will feel.
- At home activities
It is important that your home is set up appropriately for your return. Such as having commonly used things in an easily accessible place. The furniture should be moved around so that you can navigate around with a walker if needed. All rugs or throws on the floor that can be tripped on should be removed. Sitting in a higher chair and always using a chair with arm rests. A chair in the shower is also very helpful.
- Resumption of activities
We encourage walking as much as you like, but we also really like swimming, once the sutures are out and the wound is dry (around 4 weeks) and cycling on a stationary bicycle.
Activities Post Knee Replacement: http://orthoinfo.aaos.org/topic.cfm?topic=A00357
- Follow-up
You will be seen at 2 weeks, 6 weeks, 6 months, 1 year, 2 years and then every few years as needed. Often a walker or crutches are needed for up to 6 weeks. The first few weeks can be a little daunting. The wound is checked at 2 weeks, at which point it can often be a bit sensitive still. At the 6 week point, pain starts to settle. By the 6 month mark, the knee is more free, but it does not reach its maximum for up to 1 year. It is important to understand that there are always outliers. Often people will say they had no pain since 6 months others are still sore at 1.5 years. These are all within normal bounds. Pain beyond 2 year needs to be fully investigated. However most people will be resuming all normal activities by 6 months.
- Sports
Some people are keen to play sports afterwards. It is important to know that it is your knee and you can do what you like with it. However, it is important to know that it is a mechanical device and it can wear out. The more you use it, the quicker it will wear out. In general I would not recommend regular high impact sporting activities such as running or tennis. However the occasional game now and then is fine. Cycling and swimming are good ways to keep fit.
- Complications
Complications are an inevitable possibility with such a large operation. Thankfully complications are rare. As a surgeon we strive to minimize these risks, but they are still possible. It is through auditing that we are aware of our own complications so that we can be aware of our rate and keep them within or less than international levels.
- Infection 0.4 – 1%
- Blood Clot 1.36%
- Fracture
- Loosening of implant
- Patellofemoral problems (knee cap)
- Bleeding
- On-going Pain 19%*
- Peroneal nerve palsy
- Vascular Injury
- Stiffness
- Knee instability
- Other
*RB Borne et al. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not. Clin Orthop Relat Res. 2010 Jan;468(1):57-63.
http://www.ncbi.nlm.nih.gov/pubmed?term=19844772
Knee Replacement: http://orthoinfo.aaos.org/topic.cfm?topic=A00389
Arthroscopy
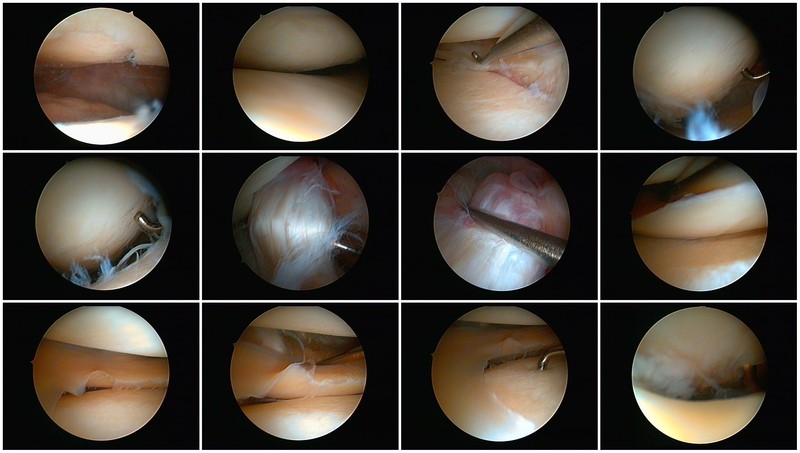
There is a complex system of soft tissue components of the knee which can cause a large array of symptoms. From a locking with a meniscal tear to general aching in the first stages of degeneration, knee arthroscopy is a relatively small procedure that is quick and easy to perform where a diagnosis and basic treatment can be instigated at the same time.
Surgery is done through 2 or more tiny stab wounds around the knee and a small fiber-optic scope is placed into the knee. This is day case surgery, where you come in that day and leave that day. Often you will have crutches to go home on and the knee can ache a bit that night, thus simple pain relief is given.
Arthroscopy is very good in that direct visualization of the anatomy can be under taken and correction performed as needed.
Typical photos taken from inside the knee.
Knee Arthroscopy: http://orthoinfo.aaos.org/topic.cfm?topic=A00299